Too much sodium is called "hypernatremia." It is from losing more water than sodium or gaining more sodium than water. Hypernatremia is diagnosed by a sodium level of more than 145 mEq/L. This, combined with low extracellular volume is called clinical dehydration. To treat hypernatremia, give the patient lots of water, as well as isotonic and hypotonic fluids which will rehydrate the cells. When a person has hypernatremia, they get a fever and postural hypotension (their blood pressure drops significantly when they stand up) as well as other symptoms.
 |
| Causes of hypernatremia Mnemonic |
 |
| Signs and symptoms of hypernatremia |
Hyponatremia is low sodium levels. It is caused by drinking too much water and not enough sodium. Hyponatremia is diagnosed as a sodium level less than 135 mEq/L. When a person has hyponatremia, they become confused. and have nausea and vomiting. Treatment for hyponatremia is hypertonic IV solutions and salt.
 |
| Hee, hee, hee |
Next is hypokalemia from low potassium levels. Diagnosis of hypokalemia comes from potassium levels less than 3.5 mEq/L. It can be caused by not eating enough potassium. The most common symptoms are muscle weakness (which can lead to the respiratory muscles as well), cramping, and constipation. It can be fixed by eating bananas, potatoes, and a few other foods with potassium levels. Some people recommend eating a mustard packet if you have a muscle cramp because there is 7mg of potassium in 1 tsp of mustard. However, a banana is a better option because bananas have 422mg of potassium per banana. Your choice. :-D
Potassium is extremely important for your heart as well. Low potassium levels can cause severe heart problems.
Hyperkalemia is high potassium levels, greater than 5.5 mEq/L. It can be caused by many different disorders, from medications to renal failure. It also has symptoms such as muscle weakness but instead of constipation, like hypokalemia, patients with hyperkalemia have diarrhea.
 |
| Causes of Hyperkalemia |
Low calcium, hypocalcemia, is next. This can be caused by not taking enough calcium or from poor vitamin D levels. Calcium can only be absorbed if there is good vitamin D levels. Signs and symptoms of hypocalcemia are numbness and tingling in the fingers, muscle twitching and contracting, and cardiac dysrhythmias. It can be diagnosed with calcium levels less than 8.4 mg/dL. It can be treated by increasing the patient's vitamin D levels as well as having them eat dairy or broccoli.
 |
| Signs and symptoms of hypocalcemia |
Hypercalcemia is calcium levels greater than 10.5 mg/dL. It can cause lethargy, confusion, cardiac dysrhythmias, and constipation. Causes of hypercalcemia are:
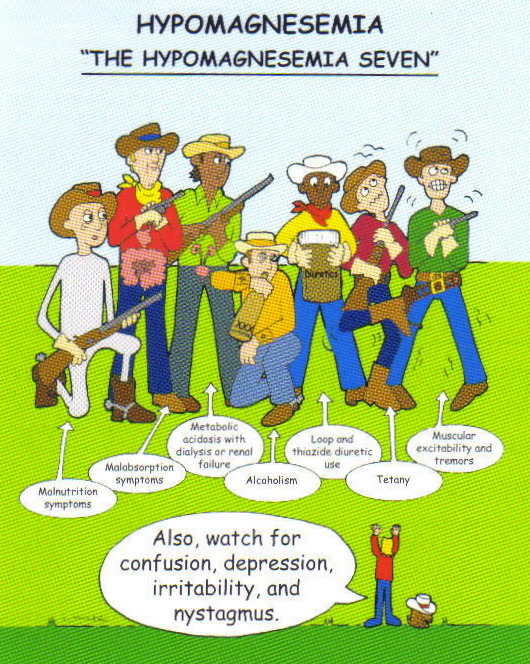
Hypomagnesemia is from low magnesium levels (less than 1.5 mEq/L). Signs of hypomagnesemia are muscle cramps, insomnia, muscle twitching, and difficulty swallowing.
The final one I'll burden you with is hypermagnesemia, or magnesium levels above 2.5 mEq/L. The common signs are lethargy, slow heart rate, muscle paralysis, and decreased respirations.
Sorry, I couldn't find any pictures to illustrate hypermagnesemia, so here's a picture of an funny cat instead:
My second test is Monday! The material for this test is much harder than the first test! Study, study, study! That's all I do anymore...At least the information is (usually) interesting!
 |
| ...I wish... |
...Until next week!










.jpg)